Conjuntos digitales militares para exteriores, uniformes militares de talla grande, traje táctico de alta calidad, equipo de caza al aire libre, novedad de EE. UU. - AliExpress

Hombre Apuesto En El Camuflaje Italiano Con Uniforme Militar Colorante Vegetato Digital Imagen de archivo - Imagen de primer, ejército: 174038621

Amazon.com: Uniforme militar, traje de camuflaje militar, ropa de paintball de camuflaje militar, Desierto digital, S : Deportes y Actividades al Aire Libre

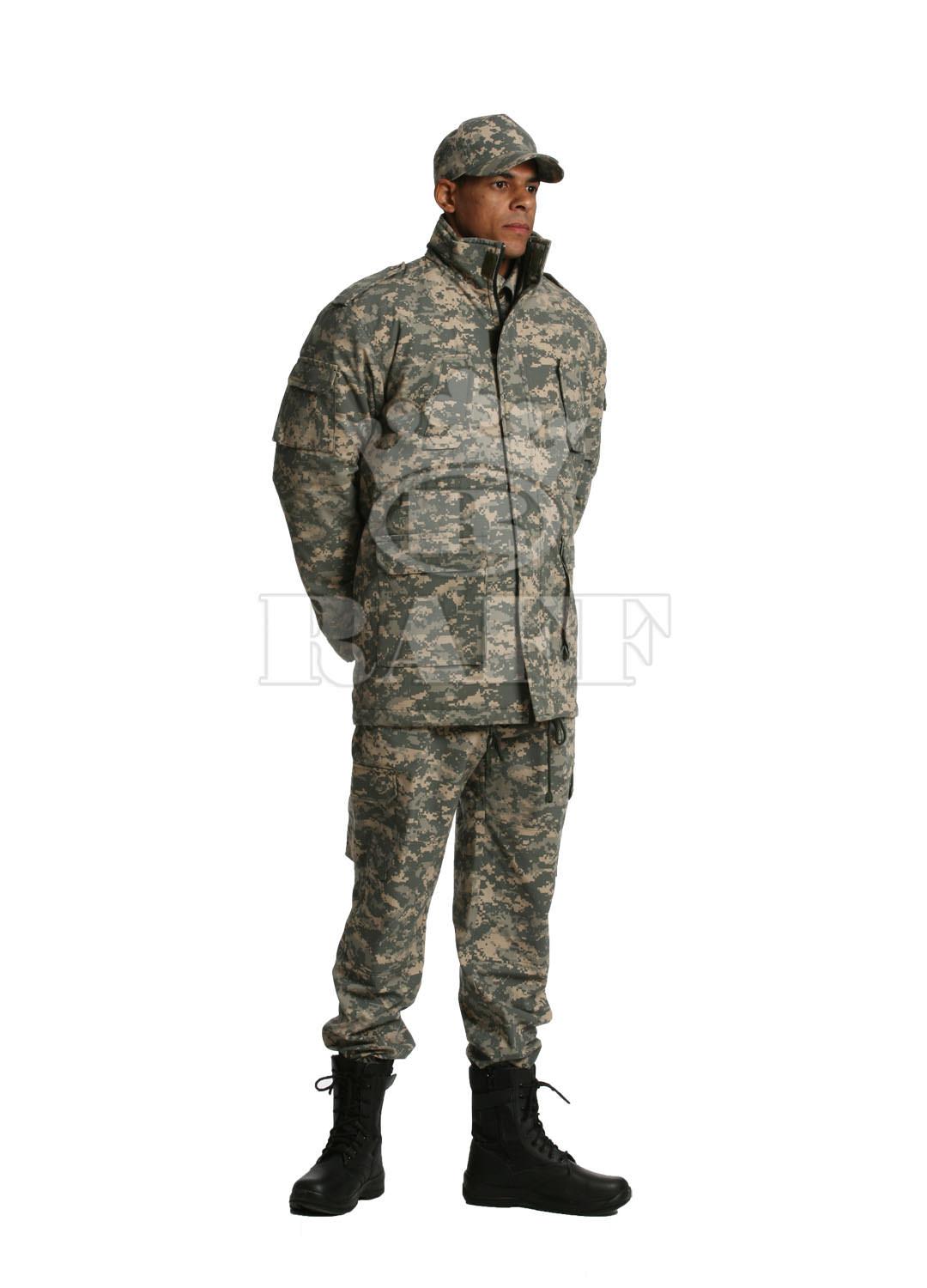
China Militares De Combate Del Ejército Uniforme ACU Digital De Color Woodland Manfuacturer & Factory | Xinxingarmy.com

China Fabricantes, proveedores de uniformes de combate del ejército de estilo militar de EE. UU. - Venta al por mayor directa de fábrica - GRUPO HENGTAI
Soldado militar del ejército ucraniano en uniformes de píxeles digitales y casco de combate | Foto Premium

Fuerzas Armadas unifican su uniforme de faena militar popularmente conocido como “chamaco” - N Digital

China Militares En Uniforme De Combate ACU Digital De Color De Camuflaje Del Desierto Manfuacturer & Factory | Xinxingarmy.com