Amazon.com: Kenworth W900 - Réplica de camión fundido a presión - Cama plana con carretilla elevadora, escala 1:32, modelo # SS10263A : Arte y Manualidades

⚠️RC TRUCKS AND MACHINES🔥Camiones Rc zona centro comercial Tres Aguas🚦CONCENTRACIÓN CAMIONES TOP - YouTube

Tractomula a control remoto, Blue Block, frecuencia 2.4 GHz, con luces LED, trailer y helicóptero, color rojo - Simaro.co

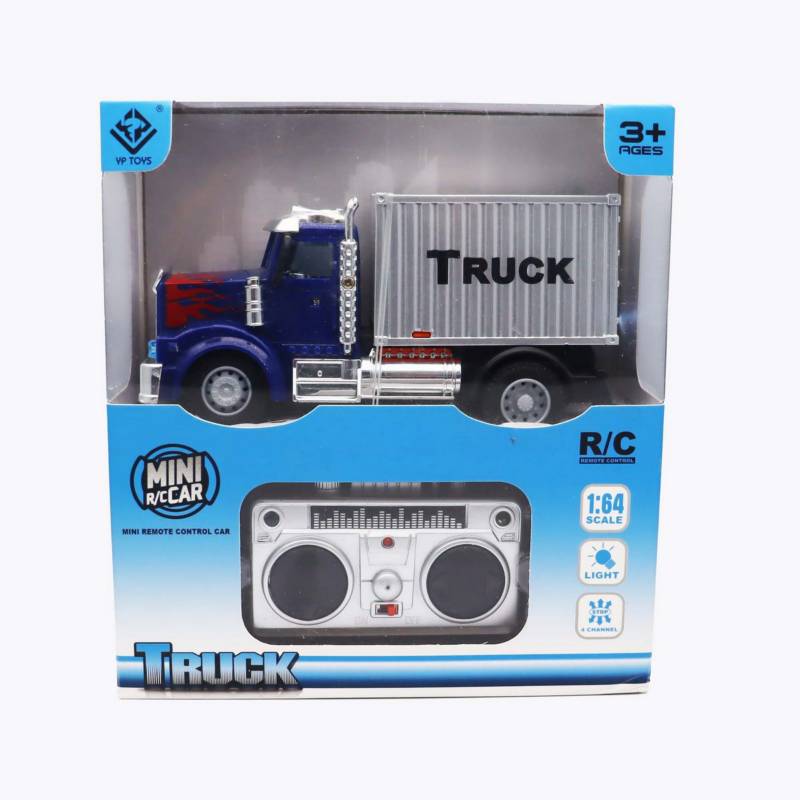
TRACTOMULA A CONTROL REMOTO - Juguetes Buffalo | Juguetes en Medellín | Juguetes en Antioquia | Juguetes en Colombia | Juguetes en Itaguí | Juguetería