Vásárlás online Zanzea hivatal női blúz, fodros alkalmi felsők tavaszi hosszú ujjú fehér blúzt elegáns fodorral blusa női ol ingre chic7 | Női ruházat \ Kinalat-Penz.cyou

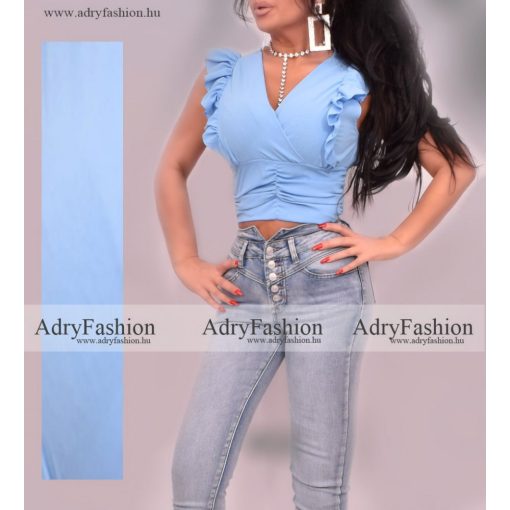
Conmoto Alkalmi V-nyakú Fodros Női Póló Nyári Egyszerű, Egyszínű Közepes Hosszúságú Felső Női Felsők, Rövid Ujjú Női Felsők Kiárusítás < Maximum & Tees | Mprice.shop

Női nyári egyszínű fodros, rövid ujjú kerek nyakú női póló, póló felső \ Női ruházat - Elemeket-Kedvezmeny.cam