
Casti wireless stereo, in-ear, incarcare rapida, 40mAh, 20-20.000 Hz, auriu rose, Silvercrest - eMAG.ro

Casti wireless Bluetooth, SilverCrest, cu design ergonomic, incarcare wireless, cu control vocal prin Siri sau Google Assistant, compatibil Android si IOS - eMAG.ro

LIDL aduce în magazine începând de joi căști true-wireless in-ear marca Silvercrest; Iată cât vor costa

Casti wireless stereo, in-ear, incarcare rapida, 40mAh, 20-20.000 Hz, auriu rose, Silvercrest - eMAG.ro

Casti wireless Bluetooth, SilverCrest, cu design ergonomic, incarcare wireless, cu control vocal prin Siri sau Google Assistant, compatibil Android si IOS - eMAG.ro
:format(webp):quality(90)/https://www.impact.ro/wp-content/uploads/2021/07/lidl-1.jpg)
Lidl dă lovitura cu un nou produs căutat de toată lumea. Căştile cu bluetooth, la un preţ fără egal - IMPACT.ro

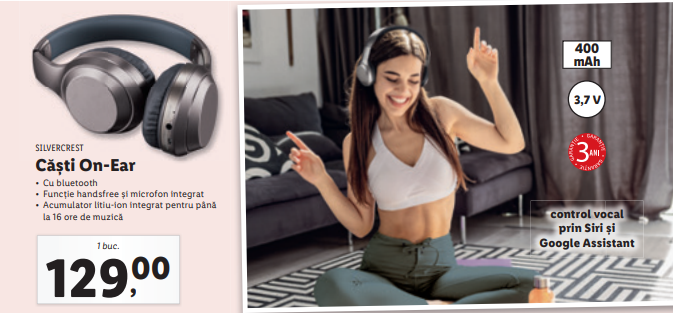
Casti wireless Bluetooth, SilverCrest, cu design ergonomic, cu control vocal prin Siri sau Google Assistant, compatibil Android si IOS - eMAG.ro

Casti Bluetooth Silvercrest - Gadgets/Casti/Camere foto-video - GREG: anunturi online gratuite de toate, pentru toti








:format(webp):quality(100)/https://www.go4it.ro/wp-content/uploads/2021/07/353844_02.jpg)


:format(webp):quality(100)/https://www.go4it.ro/wp-content/uploads/2021/12/casti2-lidl.jpg)


