Portálzár komplett szett - Kapukeret, zár, zárbetét, kilincs, zárfogadó lemez | Metal-Webshop kovácsoltvas webáruház

Weboldalunk használatával jóváhagyja a cookie-k használatát a Cookie-kkal kapcsolatos irányelv értelmében. További információk Bezár Tools Belépés Felhasználói név Jelszó Belépek Regisztrálok | Elfelejtett jelszó Keresés Az Ön Kosara Üres WebShop ...

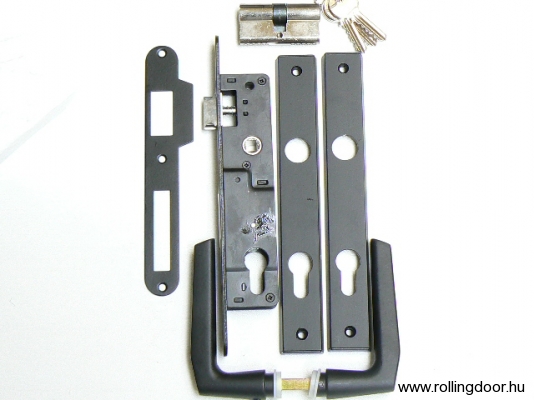
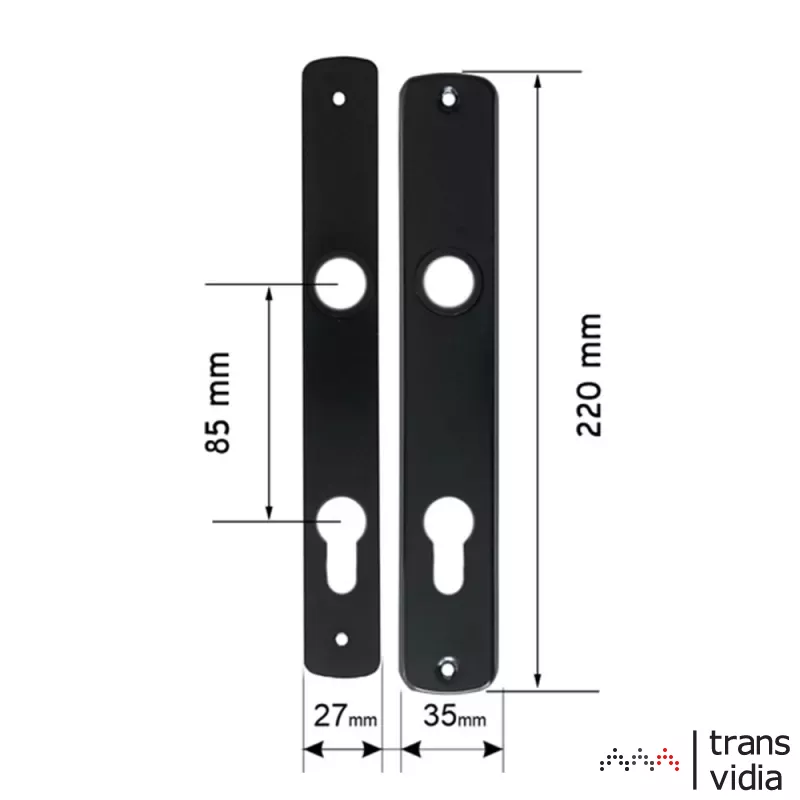
portálzár szett (Elzett zár + zárbetét + ajtókilincs 410 címmel zárólemezzel) fekete - JKH SHOP - Otthon, Kert, Barkács webáruház