Amazon.com: SAMSUNG (MB-ME256GA/AM) 256GB 100MB/s (U3) MicroSDXC EVO Select Memory Card with Full-Size Adapter : Electronics

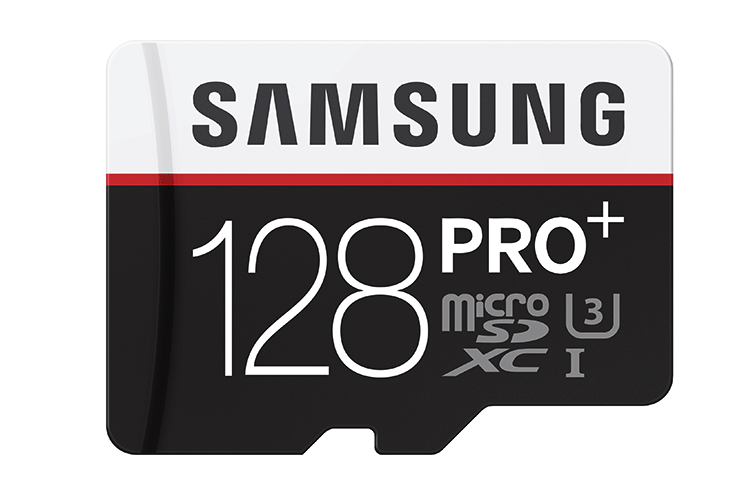
بطاقة ذاكرة سامسونج 32G 64G 128G 256G مايكرو SD SDHC SDXC الدرجة EVO + الفئة 10 C10 UHS TF بطاقات SD شحن مجاني | صفحة التفاصيل :: Thedd

Samsung EVO Select مقابل SanDisk Extreme: ما هي بطاقة الذاكرة التي يجب عليك شراؤها؟ - سامسونج | شهر فبراير 2022

بطاقة ذاكرة 256 جيجا بايت Samsung Evo Plus Micro SD XC Class 10 UHS-1 256G لهاتف Samsung Galaxy S8, S8+, Note 8, S7, S7 Edge مع قارئ USB SD/TF وWisla Trust Lanayrd(MB-MC256GA) :

تقدم سامسونج للإلكترونيات بطاقة EVO Plus سعة 256GB MicroSD ، مع أعلى سعة في فئتها 26 مايو 2016 | Samsung LEVANT_AR

Samsung Begins Mass Production of Industry's First 12Gb LPDDR5 Mobile DRAM for Premium Smartphones – Samsung Global Newsroom

ميزة زيادة ذاكرة الوصول العشوائي الرام في هواتف سامسونج ستصل للمزيد من الأجهزة قريبًا | موقع رقمي Raqami TV