
Nike Air Force 1 Shadow trainers in pastel | ASOS | Nike air shoes, Nike shoes air force, Custom nike shoes
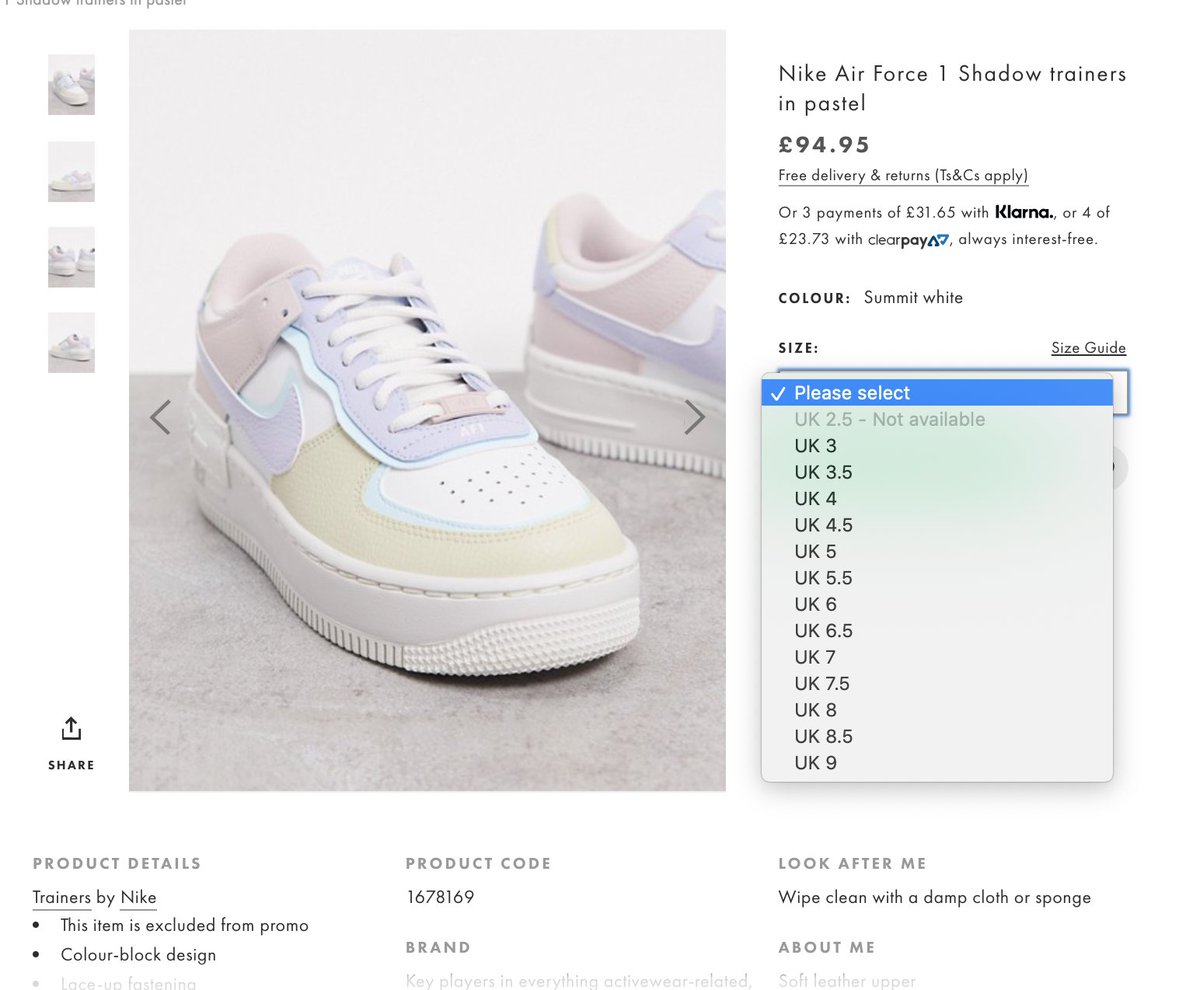
The Sole Restocks on Twitter: "Nike Air Force 1 Shadow Pastel FULL SIZE RUN restock at ASOS! Be quick... Link > https://t.co/anYtyUg6we https://t.co/UL2MN9SlB1" / Twitter






















