Dywan Paris 1350 beige+cream » Dywany akrylowe » Dywany :: Dywany24 - Dywan to komfort i wygoda! Sklep Internetowy i Salon - Wrocław

Nowoczesny akrylowy dywan Viva Acrylic 03355K L.BEIGENowoczesny akrylowy dywan Viva Acrylic 03355K L.BEIGE akryl pudrowy róż beż beżowy carpets24 carpets24pl

Nowoczesny akrylowy dywan Viva Acrylic 03352K BEIGENowoczesny akrylowy dywan Viva Acrylic 03352K BEIGE akryl brąz beż beżowy carpets24 carpets24pl

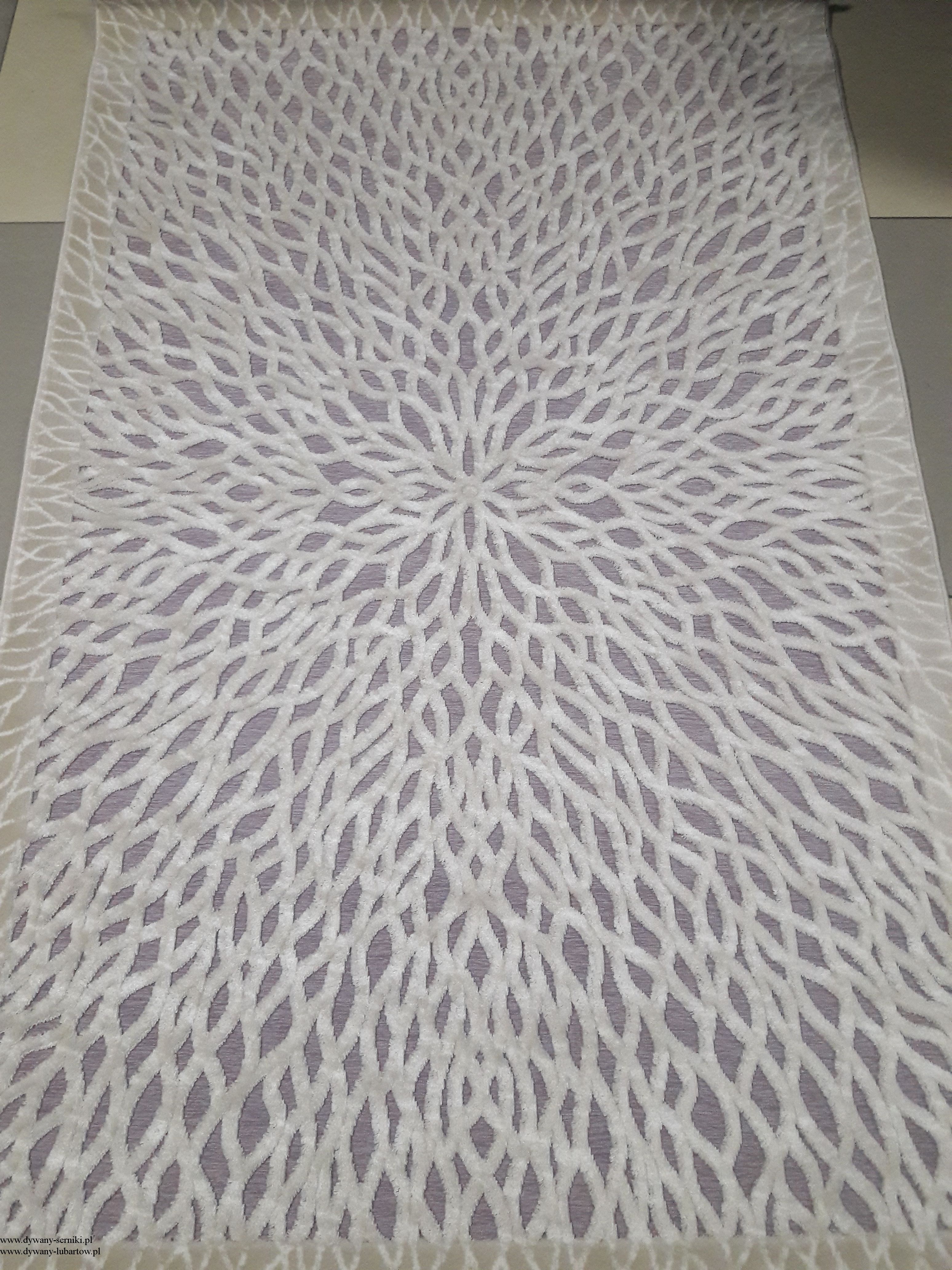
Nowoczesny akrylowy dywan Viva Acrylic 03355K Szary A.GRINowoczesny akrylowy dywan Viva Acrylic 03355K Szary A.GRI akryl szary carpets24 carpets24pl