Bestway Szolár Medence Melegítő Szőnyeg-Napenergiával-171 x 110 cm – Elektromos kisautók, akkumulátoros kisautók gyerekeknek …
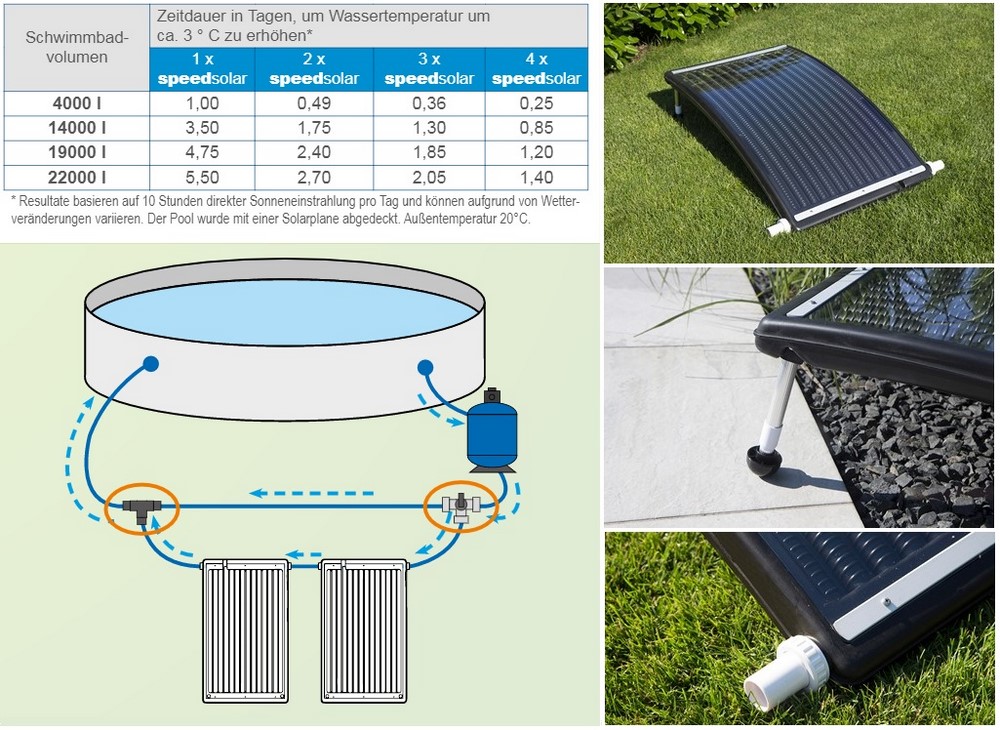
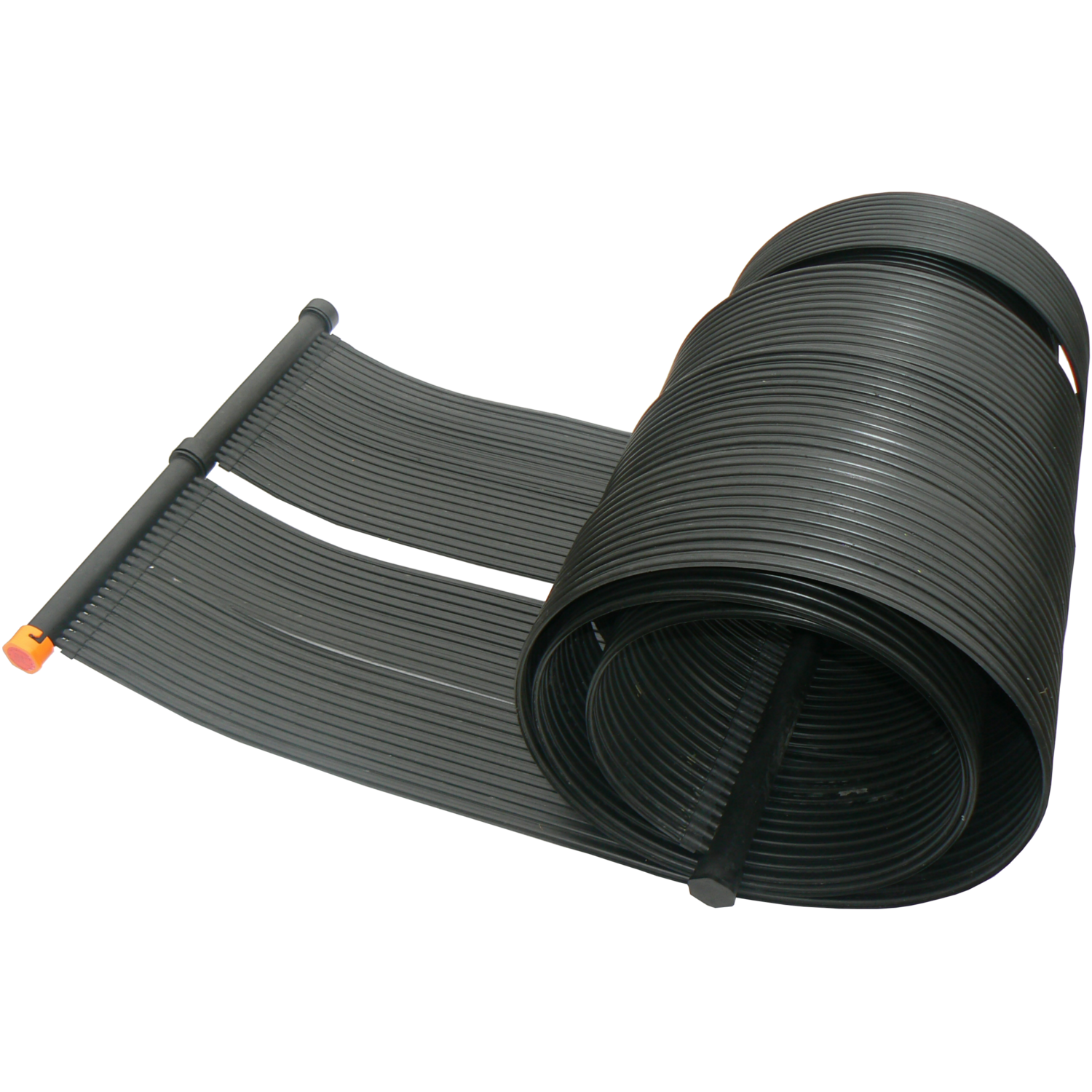
Steinbach Speedsolar HDPE szolár vízmelegítő 049106 -Medence Shop - Infotech Kft. - webáruház, webshop

Steinbach Speedsolar HDPE szolár vízmelegítő 049106 -Medence Shop - Infotech Kft. - webáruház, webshop