1 PC 4497120180 449 712 018 0 ABS Sensor Truck ABS Connecting Cable 1.8M for WABCO|wabco cable|wabco abs sensorwabco abs - AliExpress

89543 0D040 89542 0D040 ABS SPEED SENSOR, FRONT LH RH 895430D040 895420D040 SENSOR, SPEED FRONT LH RH NEW|Alternator & Generator Parts| - AliExpress

8D0927803D , VW PASSAT első abs jeladó , skoda superb abs jeladó , Audi A4 első abs jeladó , 8D0 927 803 D ,

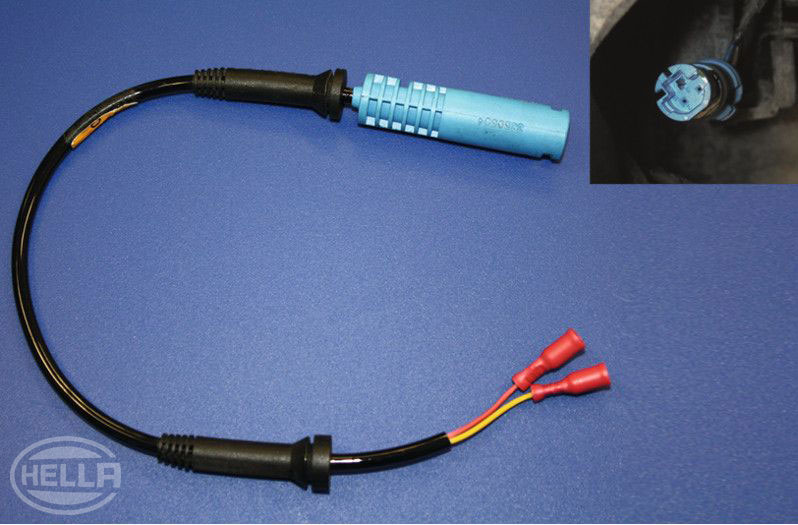
MERCEDES-BENZ ABS/EPB kabel wiring for MERCEDES-BENZ Actros truck for sale Netherlands Lemelerveld, FW13632