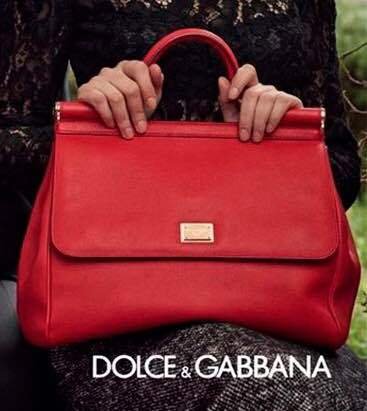
Primo Piano • Miss Sicily di Dolce&Gabbana: 20 anni e non sentirli. Dal 2009 ad oggi: design e stile di una borsa intramontabile

Primo Piano • Miss Sicily di Dolce&Gabbana: 20 anni e non sentirli. Dal 2009 ad oggi: design e stile di una borsa intramontabile