Boxe Active Profesionale Vlliodor, Putere 640 W, Microfon Wireless, Karaoke, Conectivitate prin functie Bluetooth, Port USB, Incinta Lemn, Cablu de legatura, Radio FM, Negru - eMAG.ro

Set Boxe Active Profesionale 7S-2035 800W, 15INCH, Bluetooth, USB, RadioFM, Ecran LCD, CADOU Microfon Profesional

Boxe Profesionale Vlliodor/NRS Active, Power Sound, Putere 800W, Conectivitate prin functia Bluetooth, Port USB, SD Card, Design Modern, Negru - eMAG.ro

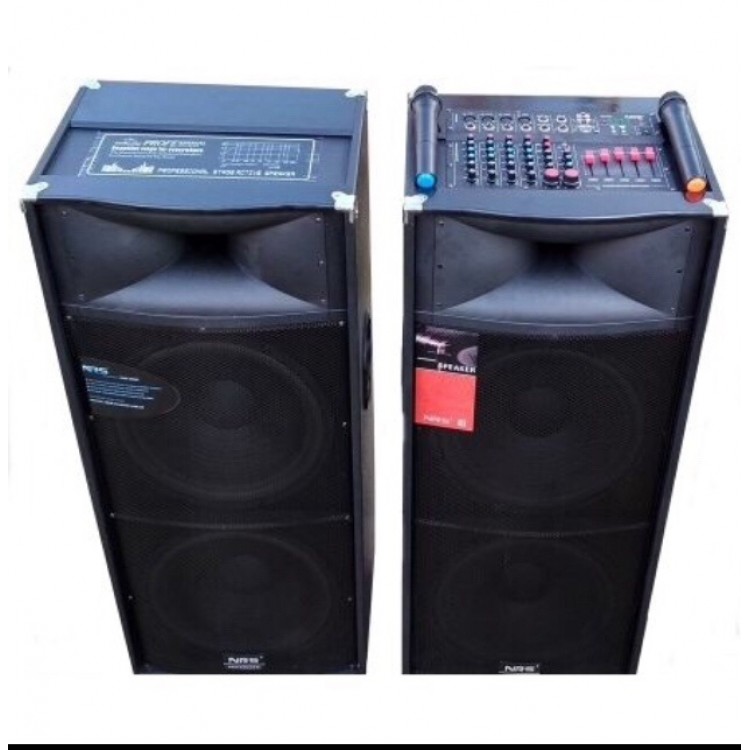
Set de 2 Boxe Active Vlliodor NRS, Putere RMS 920 W, Conectare prin Functia Bluetooth, Putere P.M.P.O 1120 W RMS, cu Mixer Puternic, Design Elegant si Materiale Rezistente,Culoare Negru - eMAG.ro

Set Boxe Active Profesionale 7S-2035 800W, 15INCH, Bluetooth, USB, RadioFM, Ecran LCD, CADOU Microfon Profesional

Set Boxe active 800 W profesionale Vlliodor 2005,15 INCH, 2 Microfoane Wireless, USB, Radio, Bluetooth - Store21

Store21.ro - 🔊 Două boxe active de 600 de W sunt pregătite și împachetate pentru următorul tău eveniment. 🔖 Economisește cu Setul de Boxe Active Vlliodor! ✓ Transport GRATUIT! ✓ Calitate garantată

Store21.ro - 💥 Set Boxe Profesionale Active Vlliodor 💥 ▫ 47% REDUCERE ▫ ✓ Putere 550W ✓ Bluetooth, Radio, Intrare USB ✓ Garanție 2 ani ➡ Comandă direct pe site: http://bit.ly/2LyriyF 📞 Comenzi telefonice la: 0762.122.221 | Facebook