2/3pcs Klasičnih Damask tiskanje Evro posteljnina nabor retro slogu doma posteljno perilo, rjuhe kritje komplet Posteljnino postelja Kritje posteljo nastavite Prevleke Akcija > Posteljnina / www.apok.si

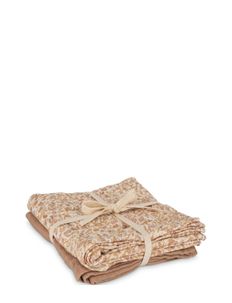
Høie of Scandinavia Winnie Sateen Bedlinen (Burned Yellow), (31.60 €) | Large selection of outlet-styles | Booztlet.com